WHAT IS RABIES???
- Rabies is a viral disease that causes acute encephalitis in warm-blooded animal. The disease is zoonotic, meaning it can be transmitted from one species to another, such as from dogs to humans, commonly by a bite from an infected animal. For a human, rabies is almost invariably fatal if post exposure prophylaxis is not administered prior to the onset of severe symptoms. The rabies virus infects the central nervous system, ultimately causing disease in the brain and death.
- The rabies virus travels to the brain by following the peripheral nerves. The incubation period of the disease is usually a few months in humans, depending on the distance the virus must travel to reach the central nervous system. Once the rabies virus reaches the central nervous system and symptoms begin to show, the infection is virtually untreatable and usually fatal within days.
- Early-stage symptoms of rabies are malaise (discomfort or uneasiness), headache and fever, progressing to acute pain, violent movements, uncontrolled excitement, depression, and hydrophobia (difficulty swallowing, shows panic when presented with liquids to drink, and can’t quench its thirst). Finally, the patient may experience periods of mania (elevated or irritable mood) and lethargy, eventually leading to coma. The primary cause of death is usually respiratory insufficiency.
- Rabies causes about 55,000 human deaths annually worldwide. 95% of human deaths due to rabies occur in Asia and Africa. Roughly 97% of human rabies cases result from dog bites (urban rabies) Infected bats, monkeys, raccoons, foxes , skunks, cattle, wolves, coyotes, dogs, mongooses (normally yellow mongoose)or cats present the greatest risk to humans (Sylvan rabies).
- In the United States, animal control and vaccination programs have effectively eliminated domestic dogs as reservoirs of rabies. In several countries, including Australia and Japan, rabies carried by terrestrial animals has been eliminated entirely. While classical rabies has been eradicated in the United Kingdom, bats infected with a related virus have been found in the country on rare occasions.
Signs and symptoms
- The period between infection and the flu-like symptoms is typically 2 to 12 weeks, but incubation periods as short as four days and longer than six years have been documented, depending on the location and severity of the inoculating wound and the amount of virus introduced. Soon after, the symptoms expand to slight or partial paralysis, anxiety, insomnia, confusion, agitation, abnormal behavior, paranoia (thought process believed to be heavily influenced by anxiety or fear), terror, and hallucinations, progressing to delirium. Rabies has been called hydrophobia because victims, locally paralyzed and unable to swallow, have been known to become agitated at the sight of water.
- Death almost invariably results 2 to 10 days after first symptoms. Once symptoms have presented, survival is rare, even with the administration of proper and intensive care. In 2005 Jeanna Giese, the first patient treated with Milwaukee protocol, became the first person ever recorded to have survived rabies without receiving successful post exposure prophylaxis. An intention to treat analysis has since found this protocol has a survival rate of about 8%.

Diagnosis
- Rabies can be difficult to diagnose, as in the early stages it is easily confused with other diseases or aggressiveness. The reference method for diagnosing rabies is by performing PCR or viral culture on brain samples taken after death. The diagnosis can also be reliably made from skin samples taken before death. Diagnosis can be made from saliva, urine, and cerebrospinal fluid samples, but this is not as sensitive. Cerebral inclusion bodies called Negri bodies(Negri bodies are eosinophilic, sharply outlined, inclusion bodies (2–10 micrometer in diameter) found in the cytoplasm of certain nerve cells containing the virus of rabies, especially in hippocampus. Often also found in the cerebellar cortex of postmortem brain samples of rabies victim) are 100% diagnostic for rabies infection but are found in only about 80% of cases. If possible, the animal from which the bite was received should also be examined for rabies.
- Cheaper rabies diagnosis will become possible for low-income settings: accurate rabies diagnosis can be done at a tenth of the cost of traditional testing using basic light microcopy and fluorescent antibody techniques.
Prevention
The vaccine is the human diploid cell vaccine (HDCV).
- Post exposure prophylaxis
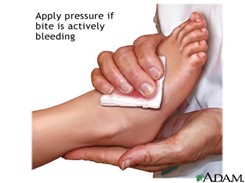
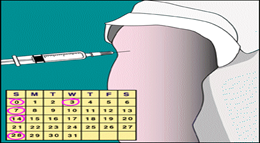
Five 1.0 ml doses of HDCV should be given intramuscularly; the first dose is given on the day 0 and is followed by the injections on day 3, 7, 14, 28. Reaction to the vaccination is uncommon. The wound should be cleaned carefully with soap and water and left open. Human rabies immunoglobulin should be given immediately (20 IU/kg); half should be injected around the area of the wound and the other half should be administered intramuscularly.
Passive Immunization
- Human Rabies Immunoglobulin HRIG
- High Risk bitten on face and neck
- Given a dose of 20 IU /Kg wt.
- Half at the site of bite and rest IM route.
- Active immunization should be initiated with passive immunization.

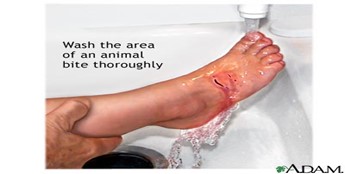
- If you are bitten or scratched

- Tell a health care worker immediately
- Wash the wound out with soap and water
- Inform the doctor right away
POSTEXPOSURE PROPHYLAXIS
1 – Wound cleaning & treatment

2- The vaccination is given on 0, 3, 7, 14, 30, and 90th day. Immunity lasts for 5 years. Injected on deltoid region IM/SC Not to be given in the gluteal region

3 – Active immunization
- Pre exposure prophylaxis
This is given to the individuals with the high risk of contracting rabies, such as laboratory workers, animal handlers and veterinarians. Two doses of HDCV 1.0 ml deep subcutaneously or intramuscularly given 4 weeks apart should provide effective immunity. A reinforcing dose are given after 12 months, and additional reinforcing doses are given every 1-3 years depending upon the risk of the exposure.
September 28 is World Rabies Day, which promotes the information, prevention, and elimination of the disease.
- Preexposure vaccination
Indicated in
- Laboratory workers.
- Veterinarians and technical staff.
- Bat handlers.





