Intravenous Anesthetics
Intravenous anesthetics are a group of fast-acting compounds that are used to induce a state of impaired awareness or complete sedation. Commonly used Intravenous anesthetics include Propofol ,etomidate, ketamine and barbiturates
BARBITURATES
- The three barbiturates most used in clinical anesthesia are sodium thiopental, thiamylal, and methohexital. Sodium thiopental has been used most frequently for inducing anesthesia. Thiamylal (SURITAL) is licensed in the U.S. only for veterinary use.
THIOPENTAL
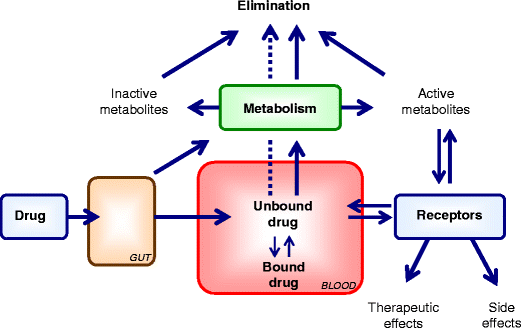
- Thiopental has very high lipid solubility, and this accounts for the speed of onset and transience of its effect when it is injected intravenously.
- The free acid is insoluble in water, so thiopental is given as the sodium salt. On intravenous injection, thiopental causes unconsciousness within about 20 s, lasting for 5-10 min.
- The anesthetic effect closely parallels the concentration of thiopental in the blood reaching the brain, because its high lipid solubility allows it to cross the blood-brain barrier without noticeable delay.
- The typical induction dose (3-4 mg/kg) of thiopental produces unconsciousness in 10-30 seconds with a peak effect in 1 minute and duration of anesthesia of 5-8 minutes.
- Recovery from the anesthetic effect of a bolus dose occurs within about 5 min, governed entirely by redistribution of the drug to well-perfused tissues; very little is metabolized in this time. After the initial rapid decline, the blood concentration drops more slowly, over several hours, as the drug is taken up by body fat and metabolized. Consequently, thiopental produces a long-lasting hangover.
- Repeated intravenous doses cause progressively longer periods of anesthesia, because blood concentration becomes progressively more elevated as more drugs accumulates in the body. For this reason, thiopental is not used to maintain surgical anesthesia but only as an induction agent.
- Thiopental binds to plasma albumin (roughly 85% of the blood content normally being bound)
- Accidental injection of intravenous thiopental-a strongly alkaline solution-around rather than into the vein, or into an artery, can cause pain, local tissue necrosis and ulceration or severe arterial spasm that can result in gangrene. If the injection is into an artery, then immediate injection of procaine, through the same needle, is the recommended procedure to encourage vasodilatation.
- Thiopental has little analgesic property and causes profound respiratory depression.
- Because intracranial pressure and blood volume are not increased (in contrast to the volatile anesthetics), thiopental is a desirable drug for patients with cerebral swelling (eg, head trauma, brain tumors).
Methohexital (barbiturate)
- Methohexital has been useful for neurosurgical procedures involving surgical removal of seizure foci. However, it also has antiseizure activity and is the drug of choice for providing anaesthesia in patients undergoing electroconvulsive therapy (ECT). Given its more rapid elimination, methohexital is also preferred over thiopental for short ambulatory procedures.
PROPOFOL
- Propofol (2,6-diisopropylphenol) has become the most popular intravenous anesthetic.
- Its rate of onset of action is like that of the intravenous barbiturates but recovery is more rapid.
- Patients feel better in the immediate postoperative period because of the reduction in postoperative nausea and vomiting and a sense of well-being.
- Propofol is used for both induction and maintenance of anesthesia as part of total intravenous or balanced anesthesia techniques and is the agent of choice for ambulatory surgery.
- Propofol has become increasingly popular for intravenous sedation in the operating room as part of a monitored anesthesia care technique and in diagnostic suites for procedural sedation.
- The drug is also effective in producing prolonged sedation in patients in critical care settings.
- Prolonged administration of conventional emulsion formulations can elevate serum lipid levels.
- Prolonged use of high dose Propofol infusions for the sedation of critically ill young children has led to severe acidosis in the presence of respiratory infections and to possible neurologic sequelae upon withdrawal.
- After intravenous administration of Propofol, the distribution half-life is 2–8 minutes, and the redistribution half-life is approximately 30–60 minutes. The drug is rapidly metabolized in the liver at a rate ten times faster than that of thiopental. Propofol is excreted in the urine as glucuronide and sulfate conjugates.
- At the usual anesthetic doses, Propofol produces dose-related depression of respiratory system.
- It also causes marked decrease in blood pressure during induction
- Pain at the site of injection is the most common adverse effect of bolus administration.
Etomidate
- Etomidate is a carboxylate imidazole that can be used for induction of anaesthesia in patients with limited cardiovascular reserve. Its major advantage over other intravenous anaesthetics is that it causes minimal cardiovascular and respiratory depression. Etomidate produces a rapid loss of consciousness, with minimal hypotension even in elderly patients with poor cardiovascular reserve. The heart rate is usually unchanged, and the incidence of apnea is low
- The drug has no analgesic effects, and coadministration of opioid analgesics is required to decrease cardiac responses during tracheal intubation and to lessen spontaneous muscle movements. Following an induction dose, initial recovery from etomidate is less rapid (< 10 minutes) compared with recovery from propofol.
- Distribution of etomidate is rapid, with a biphasic plasma concentration curve showing initial and intermediate distribution half-lives of 3 and 29 minutes, respectively. Redistribution of the drug from brain to highly perfused tissues appear to be responsible for the relatively short duration of its anaesthetic effects. Etomidate is extensively metabolized in the liver and plasma to inactive metabolites, with only 2% of the drug excreted unchanged in the urine.
- Etomidate causes a high incidence of pain on injection, myoclonic activity, and postoperative nausea and vomiting.
- It causes involuntary muscle movements during induction.
- Etomidate may also cause adrenocortical suppression with decreased plasma levels of cortisol after a single dose. Prolonged infusion of etomidate in critically ill patients may result in hypotension, electrolyte imbalance, and oliguria because of its adrenal suppressive effects.
KETAMINE
- Ketamine closely resembles, both chemically and pharmacologically, phencyclidine, which is a ‘street drug’ with a pronounced effect on sensory perception.
- The mechanism of action of ketamine may involve blockade of the membrane effects of the excitatory neurotransmitter glutamic acid at the NMDA receptor subtype
- Ketamine is a highly lipophilic drug and is rapidly distributed into well-perfused organs, including the brain, liver, and kidney. Subsequently ketamine is redistributed to less well perfused tissues with concurrent hepatic metabolism followed by both urinary and biliary excretion.
- Given intravenously, ketamine takes effect more slowly (1-2 min) than thiopental, and produces a different effect, known as ‘dissociative anaesthesia’, in which there is a marked sensory loss and analgesia, as well as amnesia, without complete loss of consciousness. During induction and recovery, involuntary movements and peculiar sensory experiences often occur.
- Ketamine produces its cardiovascular effects by stimulating the central sympathetic nervous system and, to a lesser extent, by inhibiting the reuptake of norepinephrine at sympathetic nerve terminals. Increases in plasma epinephrine and norepinephrine levels occur as early as 2 minutes after an intravenous bolus of ketamine and return to baseline levels in less than 15 minutes.
- Ketamine markedly increases cerebral blood flow, oxygen consumption, and intracranial pressure.
- Respiration is unaffected by effective anaesthetic doses. This makes it relatively safe to use in low-technology healthcare situations or in emergencies in the field.
- Ketamine is very useful for poor-risk geriatric patients and high-risk patients in cardiogenic or septic shock because of its cardio stimulatory properties.
- The main drawback of ketamine is that hallucinations, and sometimes delirium and irrational behaviour, are common during recovery.
- To enhance ketamine’s efficacy and reduce its side-effect profile, investigators separated the isomers and demonstrated that the S (+) ketamine possessed greater anaesthetic and analgesic potency. However, even the S (+) isomer of ketamine possesses psychotomimetic side effects. Ketamine has also been compounded for topical use and this preparation is purportedly useful for some types of arthritic pain.
MIDAZOLAM
- Midazolam, a benzodiazepine, is slower in onset and offset than the other intravenous anaesthetics, like ketamine, causes less respiratory or cardiovascular depression. Midazolam (or diazepam) is often used as a preoperative sedative and during procedures such as endoscopy, where full anaesthesia is not required. It can be administered in combination with an analgesic such as alfentanil. In the event of overdose, it can be reversed by flumazenil
Neuroleptanalgesia
- The combined use of a sedative (e.g., the dopamine antagonist droperidol) related to antipsychotic drugs and an opiate analgesic such as fentanyl can produce a state of deep sedation and analgesia (known as neurolept analgesia) in which the patient remains responsive to simple commands and questions but does not respond to painful stimuli or retain any memory of the procedure. This can be used for minor procedures such as endoscopy but is less used since the advent of midazolam which has a shorter duration of action. Use of neurolept analgesics is more common in veterinary medicine.